How to Produce AEP Documents & Manage Plan Benefits with Compressed Timelines
The second post in our AEP Best Practices series focuses on the critical path of the Annual Enrollment Period—how to produce AEP documents efficiently & manage plan benefits effectively with compressed timelines. It’s important to understand the risks and challenges with compressed timelines for health plans with several Plan Benefit Packages (PBPs). Here’s a graphic that lays out key milestones in the process.
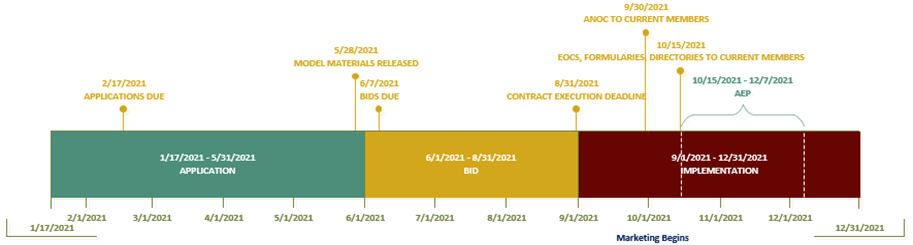
AEP Compressed Timelines
As you can see, the timeline to prepare for AEP is highly compressed. Health plans start preparing for the new contract year while still working on the previous year’s AEP. The process begins in November of the prior year with “submission of notices” of intent to apply. “Applications” are released in January and due to CMS in February. The “bid pricing tools” are released every year in April. And the next big milestone is the “submission of bids” due to CMS on the first Monday in June. Plans then work with CMS to “finalize the bid” so “contracts” can be executed by the end of August.
Lastly, all documents and functions of the approved benefit package must be completed in accordance with CMS deadlines—including the training, systems configuration, other operational processes, and documentation, as well as the marketing and communication materials noted below:
- Pre-Enrollment Materials and Sales Kits, Application Forms, and Summary of Benefits
- CMS required notices, including Enrollment/Disenrollment Notices, Appeals and Grievances Notices, Organization Determination Notices
- Outbound Enrollment Verification Letter of Script
- Member ID Card Letters and Card Templates
- Annual Notice of Change, LIS (Low Income Subsidy) Rider, Evidence of Coverage
- Provider/Pharmacy Directory and Drug Formulary
Plan Benefit Packages
For plans with several Plan Benefit Packages, the creation of PBP-specific documentation in short timeframes can be difficult. Another factor to consider is the variable environment. Data and documents go through multiple revisions before being finalized or new versions are created as updated guidance or models are released.
The PBP data is the source of numerous activities needed to implement the new contract year:
- Populating benefit information into plan documents
- Training staff on the new benefits and providing the tools and job aids needed for them to communicate this information accurately and
- Communicating with your providers and FDRs, so they have the information they need
Since this data is used in many activities, data integrity is vital to the successful and compliant launch of the new contract year. New models come out annually for some materials, and in some cases, there are corrections, or revisions to those models. A robust internal review process is essential to implement the models as they are released or revised to ensure all stakeholders are using the most recent versions. In this variable environment, compounded by compressed timelines, it’s critical Plans work efficiently and effectively to create compliant documents and processes to meet CMS deadlines.
We’re Here to Help
By leveraging the CodySoft® Collateral Management Module® and CodySoft® Plan Benefit Package Module® our health plan clients can now complete their compliant-ready documents by mid-August—substantially increasing accuracy, reducing compliance risk and eliminating stress.
In addition, CODY’s Single-Source Solution is a unique platform created to manage the entire lifecycle of Member Communications from document creation through fulfillment—including Translation Services, 508 Remediation, Provider/Pharmacy Directories, Print & Fulfillment, Electronic Fulfillment, Operations Reporting & Analytics, and a Sales & Marketing Online Ordering & Fulfillment portal.
To find out how CODY® can help your health plan operate more efficiently, mitigate risk, and deliver a better experience to serve plan members, contact us to learn more or schedule a demo.
About CODY: CODY® works with over 70 government-funded, commercial, and ACA health plans across 50 states and Puerto Rico. We help align internal operations with CMS guidelines to improve regulatory compliance, maximize performance, and streamline member/provider communications across the enterprise. CodySoft® and Membership Suite™™, our proprietary suites of software, are designed specifically for health plans. www.codyconsulting.com
