How to Ensure a Successful Triennial Network Adequacy Review
CMS monitors compliance with Network Adequacy Standards on a triennial basis. Every three years CMS requires a plan to upload its full-contract-level network into the Network Management Module (NMM) in Health Plan Management System (HPMS). When selecting contracts for the triennial review period, CMS pulls from the list of active contracts—primarily based on when the contract’s last full-network review occurred in HPMS.
CMS provides plans due for their triennial review at least 60 days’ notice to submit their networks before the deadline. Specific instructions and a specific submission timeframe are also provided for plans to submit their contracted networks. If a triggering event (see below) requires a full-network review, the plan’s subsequent triennial review timing may be reset.
Network Adequacy Criteria, Standards, and Methodology
Plans will be reviewed on standards for each county and specialty within their contracted network.
- CMS measures 27 provider specialty types and 13 facility specialty types to assess the adequacy of the network for each service area.
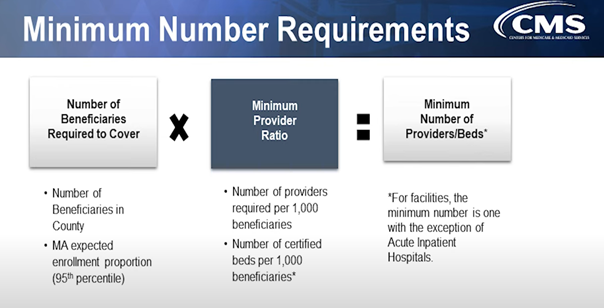
- The number of beneficiaries drives the number of providers required. Networks must be broad enough to provide enrollees residing in the county access to covered services.
- The maximum distance and travel time are based on the beneficiary and provider distribution using county type: large metro, metro, micro, rural, and counties with extreme access considerations (CEAC).
- A provider or facility must be within the maximum time and distance of at least one beneficiary to count towards the minimum number standard and may not be a telehealth-only provider.
Plans may be eligible for certain Network Adequacy credits:
- Telehealth credit: Plans may get a 10% credit towards the percentage of beneficiaries that must reside within required time and distance standards when they contract with telehealth providers in certain specialties.
- Certificate of Need (CON) Law credit: Plans may receive a 10% credit in states that have the CON laws that limit the number of providers or facilities in a county of that state.
Reference files and documents:
- The CMS supply file is a database that includes provider and facility names, addresses, NPIs, and specialty types by state and specialty type. This can be used as a resource to establish network criteria; however, it should not be the sole source of provider or facility availability in a particular service area. This file is updated annually by CMS using claims data.
- The Health Service Delivery (HSD) reference file includes network adequacy criteria for each required provider and facility type in each county. This includes the minimum provider and facility number requirements, time distance standards, ratios and criteria, and a notes tab with instructions for select specialty types. The HSD reference files are updated annually and released prior to the network reviews.
- The CON reference file lists states, counties, and specialties where states enforce CON laws or regulations. The NMM in HPMS is programmed to apply for the CON credit where applicable. Like other CMS files, the CON reference file is updated annually and released prior to the network reviews.
- HSD table instructions specify that the tables should reflect the executed contract network on the date-of-submission. Do not include providers with letters of agreement or pending contracts. A plan’s HSD table must meet the following conditions:
- Providers must not have opted out of Medicare,
- Providers are currently not sanctioned by a federal program or state licensing boards,
- Must not be pediatric providers and
- Physician Assistant and Nurse practitioner services are limited to primary care.
CMS may perform a network review after specific triggering events such as:
- Applications, initial and service area expansion (SAE)
- Significant provider/facility contract termination
- Network access complaints
- Plan-disclosed network deficiencies
Please note in CMS Rule 4192-P, beginning with contract year (CY) initial and SAE applicants would be required to submit their proposed contracted networks with the application in February. SAE applicants due for a triennial review would be required to submit their pending service area with the application in February and their existing network service areas separately during the triennial review in mid-June.
What happens if a plan fails to meet network adequacy requirements?
- During their triennial review plans may be subject to compliance or enforcement actions.
- Initial applicants may be suppressed from the Medicare Plan Finder for the upcoming Annual Election Period until the initial applicant is determined to have an adequate network in place and is prepared to provide access to service under such network in the new contract.
- Both initial and SAE applicants that fail to meet requirements by January 1 may also be subject to compliance or enforcement actions.
- Plans must ensure access to specialty care by permitting enrollees to see out-of-network specialists at the individual enrollee’s in-network-cost-sharing level for those counties/specialties that fail to have an adequate network.
- Plans may need to make alternate arrangements if the network of primary care providers is not sufficient to ensure access to medically necessary care.
We’re Here to Help
CODY® helps Medicare health plans mitigate risk and ensure their Triennial Network Adequacy Review meets CMS requirements by:
- Assessing your current operations and providing recommendations
- Working with your team to implement effective processes and internal controls
- Identifying and mitigating high-risk areas
- Conducting one-time or ongoing provider directory reviews in CMS targeted areas or across your whole network
CODY® has the team, expertise, and state-of-the-art technology to support health plan operations, improve performance, and ensure compliance with industry and regulatory standards. To learn more, contact us today.
About CODY: CODY® works with over 70 government-funded, commercial, and ACA health plans across 50 states and Puerto Rico. We help align internal operations with CMS guidelines to improve regulatory compliance, maximize performance, and streamline member/provider communications across the enterprise. CodySoft® and Membership Suite™™, our proprietary suites of software, are designed specifically for health plans. www.codyconsulting.com
